Reading time about 5 minutes.
I am not a medical professional and none of these writings should be considered as a professional or legal recommendation for treatment. Sites that are linked by Motherhood Minute are not monitored or investigated. Please refer to them at your own risk and awareness.
As discussed in my last newsletter on the cost of mental healthcare, a major hindrance to receiving care for mental health conditions includes the symptoms of those conditions themselves: brain fog, loss of motivation, and decreased feelings of self-worth. How can we make it easier for those needing help before it becomes a crisis situation?
According to a Crisis Intervention Team education module1 I found through the University of Memphis, a crisis is “short-term and overwhelming and involves a disruption of an individual's normal and stable state where the usual methods of coping and problem solving do not work.” It also means that someone experiencing a crisis feels out of control and is thinking in terms of “here and now.”
What feels striking to me, as someone who has routinely looked for means of mental health care online, is that many reputable sources (such as NAMI.org) will define a crisis as a plan of self-harm, harming others, or suicide but do not include this definition of a crisis as it is defined to crisis intervention teams!
We also know that resources like NAMI can provide descriptions of specific mental health conditions, hotlines or plan of actions for crisis situations (as described as self/other harming crises), and can give suggestions on how to handle specific life situations. These can be helpful in some cases, such as NAMI’s blog posts on handling grief, job loss, etc, but they all seem to present information with a mentally healthy person in mind.
What is the “in-between” like?
For simplification, I am furthermore going to define the “mental health gap” as the lack of care between finding professional care and being in a crisis situation.
We will define the “in-between” as the mental state an individual may feel when they are not at their normal or healthy state of mental health, but they are also not in harming crisis mode.
As someone diagnosed with major depressive disorder when they were 21 but has suffered from reoccurring symptoms since she was 11, I enjoy bringing more clarity to what depression can feel like. I find this graphic below helpful.
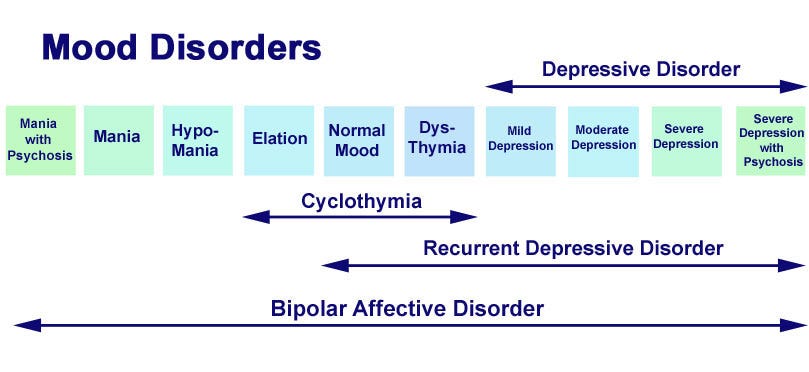
Normal in this chart refers to no major elated or depressive mood averages. On medication, my range is closer to Recurrent Depressive Disorder, but sometimes the “ normal “ baseline for me will plunge closer to moderate to severe depression; therefore, I think of my normal as the center of the spectrum based on the mood disorder displayed. Off medication, I can find myself anywhere from elation (a fun way to hyper-focus for a while) to severe depression. Before I removed substance abuse from my life, I would occasionally slip from hypomania to severe depression with psychosis.
As a result of updating the definition of a mental health crisis, the gap in care could be minimized by considering the varieties of the mood spectrum per individual. We can do better to help those in the “in-between” by writing mental health help resources from the perspectives of readers who may feel a lack of focus and need clear paths of action before they reach crisis.
Any advocacy agency or organization can take the following actions to help those seeking help.
Redefine what it means to be “in crisis” by combining the current definition with the definition provided to those studying crisis intervention.
This would be a more inclusive definition that shows the spectrum of crisis: stressful circumstances, elevated mood changes, emotional distress, mental overwhelm, and confusion about care, as well as desire/thoughts of harming oneself or others.
The proposed definition of a mental health crisis: an overwhelming state of mind that involves a disruption of an individual's normal and stable state, where the usual methods of coping and problem-solving do not work. This can be displayed differently in individuals but typically involves acute feelings of distress, which could lead to worsened symptoms involving thoughts of harm to self or others.
Redefining what a crisis is also helps individuals realize their struggles are worth receiving care when they may otherwise hesitate to define their problems as a life/death crisis. This is particularly true for those experiencing loss, those with long-term mood disorders, chronic-pain or illness patients, and pre/post partum women experiencing depression.
Eliminate using “self-care” terminology as a way to help those seeking medical mental health care. Self-care is too closely aligned with cultural and capitalist efforts to sell comfort to mass populations. (More on that later).
Offer clear action plans through easy-to-read outline formats and infographics for readers seeking help. Plan of actions may be repetitive in some instances but offering multiple phrase options that appeal to someone feeling unrelatable will help an uneasy mind navigate information-heavy resources.
Organizations often assume readers have been able to receive a diagnosis and create resources divided into categories that make sense to a medical provider, not to someone confused about their distress.
Offering chat support to those confused about what to do while they wait for professional help can give individuals immediate support while using the same techniques a crisis hotline would.
(To their credit, NAMI is already offering this with their HelpLine, although confusion to readers still remains if this is for youth ages only or includes adults in need. Another list of hotlines can be found at Project Healthy Minds, a resource created to equip corporate entities to share resources with employees better.)Create better communication pathways between therapists and primary care physicians that alert both parties of patient outreach for counseling or medication treatment. Online resources can offer to send an email notice to primary care providers if individuals spend time browsing a resource site or talking with a crisis helpline to cross the bridge between self-help and medical help. (There are situations where this could complicate legislation laws, but it’s a discussion that would be worth having between professions.)
We can create a better experience for people seeking help while they are waiting to find it. I have also created two infographics you can share. One is a generic version and the other has a space on the bottom that allows a Provider to write in their contact information if they choose to print it through Canva or another service.
Please enjoy those designs here and let me know if you have questions.
What do you think? How else can we create more accessible pathways to care?
In the coming weeks, we will continue this series on Mental Health, and I hope you consider supporting my work with Motherhood Minute as a subscriber. I also want to thank the men and women who have sent me private direct messages and emails to share their mental health treatment journeys. Thank you for your vulnerable conversations.
If you haven’t already, check out the other topics on Mental Health at Motherhood Minute here and share this newsletter with someone who could benefit from the conversation and resources. Bonus points if you share this particular conversation with your mental health care provider ;)
http://www.cit.memphis.edu/modules/De-Escalation/presentations/FL%20-%20De%20Escalation%20Techniques.pdf





I encourage anyone with ongoing mental health issues to find out if there’s a local community mental health clinic in their area. While understaffed, they often have case managers who can help guide you during those challenging times. Also, some have walk-in hours for therapy sessions and outpatient psychiatric care (regardless of one’s ability to pay). I hope this helps!
Thank you for writing about this "gap" phase when someone is having a crisis...such an important topic to spotlight.